POTELIGEO had a median time to response of about 1 month in blood1,a-g
POTELIGEO also had a median time to response of 3 months in skin
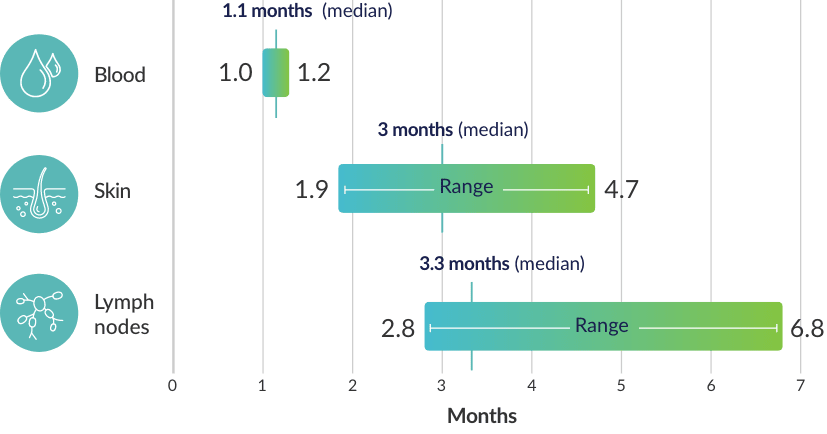
- aTime to response was measured based on a post hoc analysis; a finding from the post hoc analysis cannot be used to demonstrate differences between treatments and may not be applicable to all patients initiating POTELIGEO.
- bResponse was defined by international response criteria for Mycosis Fungoides and Sézary Syndrome.2
- cResponses in skin and blood must have persisted for ≥4 weeks to be confirmed and were evaluated every 4 weeks during treatment.3,4
- dResponses in lymph nodes were evaluated at 4 weeks, then every 8 weeks for the first year, and every 16 weeks thereafter.1
- eResponse in skin defined as ≥50% clearance of skin disease without new tumors, evaluated using the modified Severity Weighted Assessment Tool (mSWAT).4
- fResponse in blood defined as >50% decrease in high blood tumor burden (B2), assessed by central flow cytometry.4
- gResponse in lymph nodes defined as cumulative reduction ≥50% of measurable disease of each abnormal lymph node and no new abnormal lymph nodes, evaluated by computed tomography (CT) scans.4
CTCL Expert Perspectives: Treatment Considerations
Watch Francine Foss, MD, Professor of Medicine (Hematology and Dermatology) at Smilow Cancer Hospital at Yale New Haven discuss different treatment options based on staging, clinical practice guidelines, blood involvement, and patient feedback for those with Mycosis Fungoides or Sézary Syndrome.
In a post hoc analysis, POTELIGEO demonstrated a longer TTNT in patients with Mycosis Fungoides and Sézary Syndrome vs vorinostat5,h
TTNT (months), overall and by disease type5
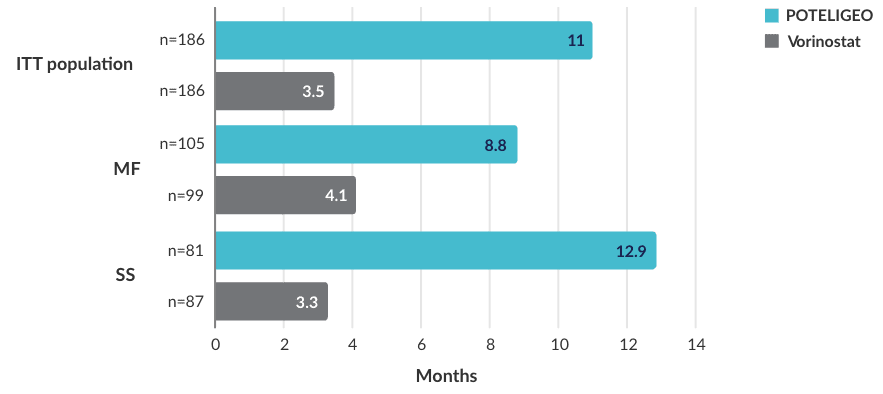
- TTNT was defined as time to any significant therapy (systemic treatment, total skin radiation, or psoralen-UVA therapy)5
- POTELIGEO also demonstrated significantly longer TTNT vs vorinostat across blood classifications6
TTNT (months), across blood classifications6
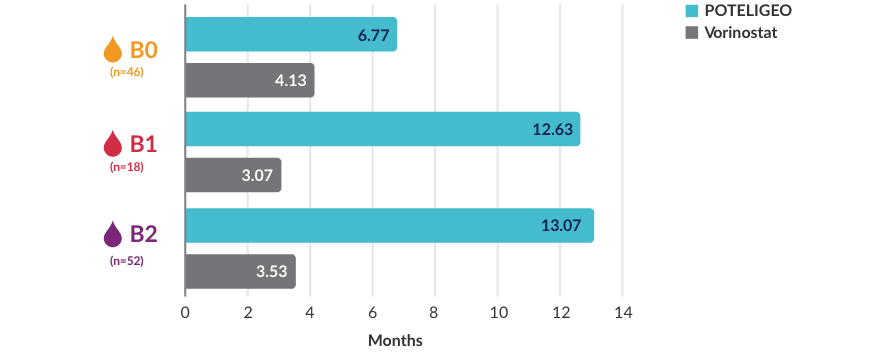
BLOOD CLASSIFICATION
-

-
<15%
CD4+CD26- or CD4+CD7-cells by flow cytometry
-

-
≥15%
CD4+CD26- or CD4+CD7- cells by flow cytometry
-

-
≥1000/μL Sézary cells with positive clone
or 1 of the following:- CD4:CD8 ratio ≥10,
- 40% CD4+CD7- cells, or
- ≥30% CD4+CD26- cells
- hFindings from the post hoc analysis cannot be used to demonstrate differences between treatments and may not be applicable to all patients initiating POTELIGEO.
- ITT=intent-to-treat; TTNT=time to next treatment; UVA=ultraviolet A
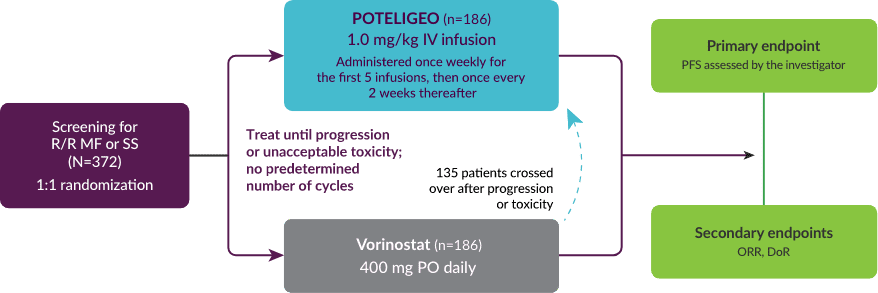
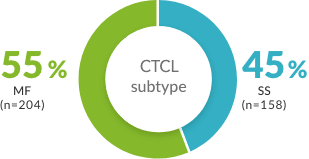
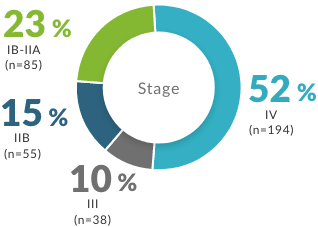
In the MAVORIC trial, POTELIGEO’s response was measured in skin, blood, and lymph nodes
See efficacy data across disease compartments- Kim YH, Bagot M, Pinter-Brown L, et al. Mogamulizumab versus vorinostat in previously treated cutaneous T-cell lymphoma (MAVORIC): an international, open-label, randomised, controlled phase 3 trial. Lancet Oncol. 2018;19(9):1192-1204.
- Olsen EA, Whittaker S, Kim YH, et al. Clinical end points and response criteria in mycosis fungoides and Sézary syndrome: a consensus statement of the International Society for Cutaneous Lymphomas, the United States Cutaneous Lymphoma Consortium, and the Cutaneous Lymphoma Task Force of the European Organisation for Research and Treatment of Cancer. J Clin Oncol. 2011;29(18):2598-2607.
- POTELIGEO [package insert]. Kyowa Kirin Inc., Princeton, NJ USA.
- Kim YH, Bagot M, Pinter-Brown L, et al. Mogamulizumab versus vorinostat in previously treated cutaneous T-cell lymphoma (MAVORIC): an international, open-label, randomised, controlled phase 3 trial. Lancet Oncol. 2018;19(9):1192-1204. Supplementary appendix published online August 9, 2018. doi.org/10.1016/S1470-2045(18)30379-6
- Kim YH, Ortiz-Romero PL, Pro B, et al. Time to next treatment in patients with previously treated cutaneous T-cell lymphoma (CTCL) receiving mogamulizumab or vorinostat: a post-hoc analysis of the MAVORIC study. Hematol Oncol. 2019;37(S2):285-286.
- Cowan R, Scarisbrick JJ, Zinzani PL, et al. Efficacy and safety of mogamulizumab by patient baseline blood tumour burden: a post hoc analysis of the MAVORIC trial. J Eur Acad Dermatol Venereol. 2021;35(11):2225-2238.
- Kim Y, Bagot M, Zinzani PL, et al. Safety of mogamulizumab in mycosis fungoides and Sézary syndrome: final results from the phase 3 MAVORIC study. Blood. 2019;134(suppl):5300[abstract].
- Data on file. Kyowa Kirin Inc., Princeton, NJ USA.